14 Apr 2025
Recommended
Minimum 30 mins
Course
Access
Certification
Voiceover
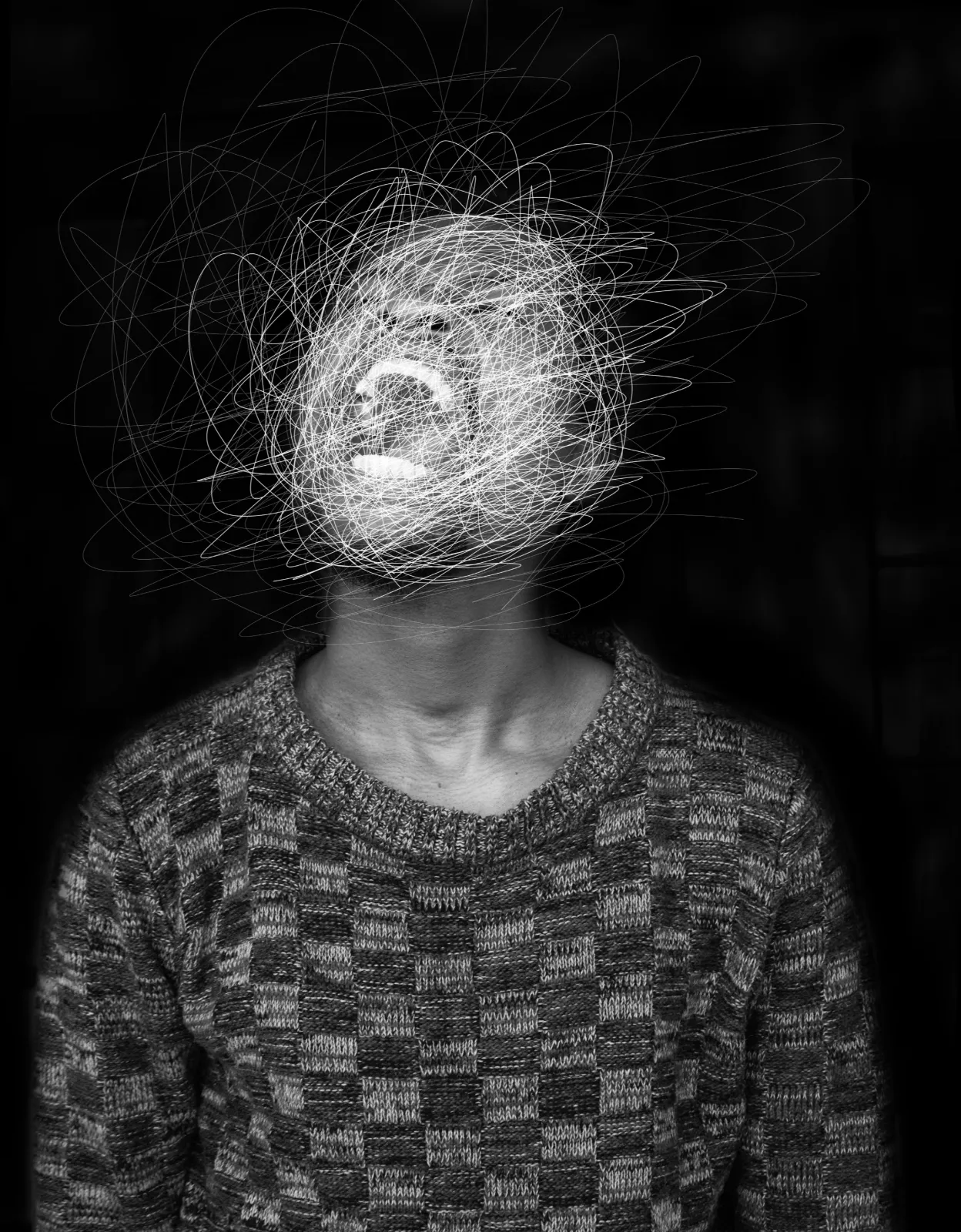
Borderline Personality Disorder (BPD), also referred to as Emotionally Unstable Personality Disorder (EUPD), is a complex and challenging mental health condition marked by emotional dysregulation, impulsive behaviour, unstable relationships, and a disturbed sense of identity.
It affects an estimated 0.7 to 2% of the UK population and is linked to significant psychological distress, impaired daily functioning, and an increased risk of self-harm and suicide. Individuals with BPD frequently access a range of healthcare services, including general practice, mental health care, and emergency departments, often during times of crisis. Therefore, it is essential for healthcare professionals to possess a clear understanding of the condition to ensure compassionate, timely, and effective support.
This course aims to provide healthcare professionals with evidence-based knowledge and practical skills to identify symptoms, conduct appropriate assessments, and implement supportive strategies, ultimately improving outcomes and promoting recovery for individuals living with BPD.

 £25
£25
Learning Outcomes.
By the end of this course,participants will be able:
To define Borderline Personality Disorder (BPD), outline its key features, discuss its prevalence in the UK, and address common myths, misconceptions, and stigma.
To recognise the core symptoms and types of BPD, understand diagnostic criteria, differentiate BPD from similar conditions, and explore the role of healthcare professionals in early identification.
To examine the biological, genetic, and environmental causes of BPD, including the impact of childhood trauma, neglect, and Adverse Childhood Experiences (ACEs), alongside neurobiological factors.
To evaluate evidence-based treatments for BPD, including when medication is appropriate, the role of psychological therapies like DBT, and strategies for crisis management and suicide prevention.
To develop skills for supporting individuals with BPD, including building therapeutic relationships, promoting coping strategies, involving family and support networks, and ensuring effective safety planning.
To understand multi-disciplinary approaches to BPD care, review UK policies on personality disorders, and identify strategies to manage burnout and access continuing professional development (CPD).
Course
Contents.
01
BPD is a complex mental health disorder marked by emotional dysregulation, impulsivity, unstable relationships, fear of abandonment, identity disturbance, and self-harming behaviours.
03
Symptoms fall into affective, impulsive, cognitive-perceptual, and interpersonal groups, with recognised subtypes such as impulsive and self-destructive BPD.
05
Causes include genetic predisposition, neurobiological dysfunction, and environmental factors, especially childhood trauma and neglect.
08
Includes suicide prevention strategies, de-escalation techniques, structured risk assessments, and the development of safety plans.

06
BPD frequently coexists with depression, anxiety, PTSD, eating disorders, and substance misuse, complicating clinical management.
09
Emphasises therapeutic relationships, effective communication, patient rights, safeguarding, family involvement, and promoting self-help strategies.
02
Affects approximately 1–2% of the UK population, with stigma and misconceptions contributing to diagnostic and treatment barriers.
04
Diagnosis relies on DSM-5 and ICD-11 criteria; accurate assessment is essential to differentiate BPD from other psychiatric conditions like bipolar disorder or PTSD.
07
Psychological therapies such as DBT, MBT, CBT, and Schema Therapy are central; medications may support symptom management but are not curative.
10
Advocates for multidisciplinary, holistic care guided by NICE and NHS policies; prioritises staff wellbeing, risk management, and ongoing professional development.
The Borderline Personality Disorder (BPD) Awareness Course provides healthcare professionals with essential knowledge on BPD symptoms, causes, diagnosis, and treatment. It addresses UK prevalence, dispels myths, and highlights the impact of stigma. The course covers evidence-based therapies, crisis and suicide prevention, and safeguarding. It emphasises multidisciplinary collaboration, trauma-informed care, and involving support networks, while offering strategies to manage professional burnout and encouraging access to ongoing continuing professional development.
 Summary
Summary


